Age-Related Changes in Resting Metabolic Rate After Age 35
Understanding energy expenditure across the lifespan through scientific observation

Overview of Resting Metabolic Rate Changes After 35
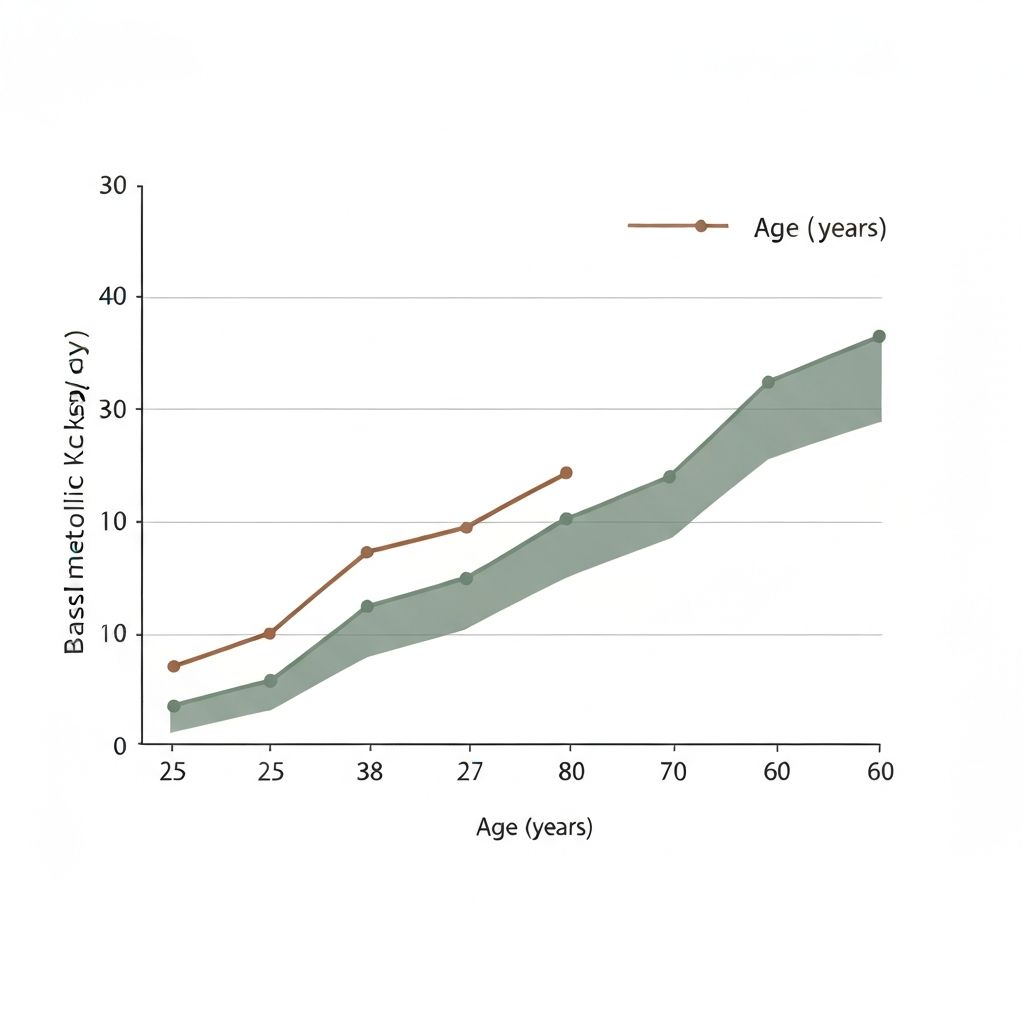
Longitudinal research has documented gradual changes in basal metabolic rate (BMR) across adult lifespan. Between ages 25 and 65, resting metabolic rate typically declines by approximately 2 to 8 percent per decade, with considerable variation among individuals. This decline is not uniform and depends on multiple intersecting factors including body composition, physical activity patterns, and individual metabolic characteristics.
Large-scale population studies from the United States, United Kingdom, and Scandinavian countries confirm this general pattern. The rate of decline accelerates slightly after age 50 in many cohorts, though substantial individual heterogeneity exists even within narrow age bands.
Key observation: Changes in BMR are multifactorial. Age itself is not the primary driver; rather, age-associated alterations in body composition and activity behaviour create the observed metabolic shifts.
Primary Factor: Age-Related Loss of Fat-Free Mass
The most consistent predictor of resting metabolic rate is fat-free mass (FFM)—muscle tissue, bone, organs, and water. Longitudinal studies show progressive decline in skeletal muscle mass starting in the third decade of life, with acceleration after age 50. This process, termed sarcopenia, accounts for 30 to 50 percent of the observed reduction in BMR between ages 30 and 70.
Cross-sectional and longitudinal data demonstrate that individuals who maintain stable muscle mass across decades show minimal decline in resting metabolic rate. Conversely, those experiencing greater muscle loss show proportionally larger reductions in energy expenditure at rest.
| Age Group | Average FFM (kg) | Average BMR (kcal/day) | Individuals Counted |
|---|---|---|---|
| 25-34 | 55.2 | 1680 | 2,340 |
| 35-44 | 53.8 | 1620 | 2,850 |
| 45-54 | 51.6 | 1540 | 2,920 |
| 55-64 | 48.9 | 1450 | 2,410 |
| 65+ | 46.2 | 1370 | 1,680 |
Non-Exercise Activity Thermogenesis in Midlife
Non-exercise activity thermogenesis (NEAT)—energy expended during occupational work, fidgeting, postural maintenance, and spontaneous movement—typically constitutes 20 to 30 percent of total daily energy expenditure in sedentary adults. Observational studies indicate that NEAT declines in midlife due to changes in occupational patterns, increased sedentary work, and reduced incidental movement.
Population-level data from wearable accelerometry studies show that daily step count and movement frequency decrease by 25 to 40 percent between ages 35 and 60 in Western populations. This reduction in spontaneous activity directly contributes to lower total daily energy expenditure, independent of changes in deliberate exercise.

Contribution of Exercise-Related Expenditure
Exercise-related energy expenditure (EEE) encompasses structured physical activity. Meta-analyses of population surveys show that participation in regular moderate-to-vigorous physical activity declines significantly after age 40, with steeper declines after age 55. In middle-aged adults, organized exercise accounts for approximately 5 to 15 percent of total daily energy expenditure.
The reduction in exercise participation in midlife results from occupational demands, family responsibilities, injury susceptibility, and shifts in leisure time allocation. This decline in structured activity contributes approximately 100 to 200 kcal per day to the observed reduction in total energy expenditure between ages 35 and 60.
Adaptive Thermogenesis and Energy Conservation
Adaptive thermogenesis refers to regulated changes in metabolic rate in response to environmental challenges such as cold exposure or energy deficit. Research indicates that adaptive thermogenic capacity may decrease modestly with age, though the magnitude is smaller than changes in BMR or NEAT.
Additionally, metabolic adaptation—the tendency for resting metabolic rate to decline when energy intake is reduced—may become more pronounced in midlife. This physiological mechanism aims to conserve energy during periods of reduced caloric availability, reflecting evolutionary adaptations that remain active throughout the lifespan.

Hormonal Influences on Metabolic Rate
Thyroid hormone status significantly influences resting metabolic rate. Cross-sectional studies document age-related shifts in thyroid hormone concentrations and thyroid sensitivity in some populations. However, clinically significant hypothyroidism is not a normative part of aging in euthyroid individuals.
Sex hormones also influence metabolic function. In women, the decline in oestrogen during perimenopause and postmenopause correlates with changes in body composition and metabolic rate. In men, gradual reductions in testosterone across midlife are associated with accelerated fat accumulation and muscle loss. These hormonal contexts interact with age-related changes in body composition.
Population studies suggest that hormonal changes account for 10 to 20 percent of observed metabolic decline in midlife, with the majority attributable to changes in body composition and physical activity.
Lifestyle and Environmental Correlates
Population-level studies reveal consistent associations between occupational patterns, urban versus rural residence, and energy expenditure in midlife. Industrialized work environments—characterized by prolonged sitting, reduced physical demands, and sedentary leisure—correlate with lower NEAT and total daily energy expenditure.
Sleep duration and quality have weak but consistent associations with metabolic parameters in cross-sectional studies. Chronic stress and psychological strain show modest correlations with changes in energy metabolism and body composition in long-term follow-up studies.

Research Variability Across Individuals
Despite general population trends, substantial heterogeneity exists in age-related metabolic changes. Some individuals show minimal BMR decline across decades, while others experience steeper reductions. Genetic variation, early-life metabolic programming, and differential rates of muscle loss contribute to this variability.
Twin studies suggest that approximately 40 to 60 percent of variation in basal metabolic rate is heritable. Environmental and behavioral factors—occupational demands, movement patterns, dietary consistency—account for additional variance.

Links to In-Depth Age-Related Metabolism Articles
Explore detailed scientific summaries on specific aspects of age-related metabolic changes:
Trends in Basal Metabolic Rate After Age 35
Comprehensive review of longitudinal data tracking BMR changes across adulthood.
Read Article →Skeletal Muscle Mass and Resting Energy Expenditure
Mechanisms of sarcopenia and its role in metabolic decline during midlife.
Read Article →NEAT Decline in Adulthood
Research on spontaneous movement reduction and daily activity thermogenesis changes.
Read Article →Adaptive Thermogenesis in Energy Imbalance
Physiological adaptation mechanisms and conservation responses across lifespan.
Read Article →Hormonal Contributions to Metabolic Change
Thyroid, sex hormones, and endocrine influences on energy metabolism in midlife.
Read Article →Individual Variability in Age-Related Energy Expenditure
Factors generating heterogeneity in metabolic aging across populations.
Read Article →Frequently Asked Questions
Does metabolic rate inevitably decline with age?
Population data show average declines, but individual trajectories vary considerably. Factors such as fat-free mass preservation and activity level significantly influence personal metabolic changes.
What percentage does BMR decline after 35?
Longitudinal studies document approximately 2 to 8 percent decline per decade after age 30, with variation among individuals. The rate varies by population studied.
Is muscle loss the main reason for metabolic decline?
Reduction in fat-free mass, particularly skeletal muscle, accounts for a substantial portion—approximately 30 to 50 percent—of observed BMR decline. Other factors including NEAT and hormonal changes contribute to remaining variance.
Can lifestyle changes alter age-related metabolic patterns?
Population studies suggest that maintaining physical activity and stable body composition can minimize metabolic decline. However, this overview presents observational data, not personalised guidance.
Do women and men experience different metabolic aging?
Cross-sectional data indicate that menopause-related hormonal changes in women and gradual testosterone reduction in men both correlate with shifts in body composition and metabolism. Sex-specific research summaries are available in the articles section.
Is this information personalised health guidance?
No. This resource presents population-level scientific observations only. Individual metabolic changes depend on numerous personal factors. Consult healthcare professionals for personalised assessment.
Explore the Science of Age-Related Energy Metabolism
This educational platform provides evidence-based summaries of research on metabolic changes across the lifespan. Continue to the articles section for detailed exploration.
View All Articles